Diabetes continues to be a, “high over-all death burden” even in the year 2019. It is a serious, chronic disease, with 65% of deaths attributed to cardiovascular disease; there is an elevated risk for heart attacks, heart failure 2-5 times more, strokes and other related cardiac complications. The prevalence of obesity remains on the rise, with consequences such as the metabolic syndrome, leading to type 2 diabetes and additional medical problems. We used to think you could be healthy even with obesity; being healthy but obese, still leads to heart issues, according to a new study. Obesity can affect blood pressure, raise inflammation levels and blood sugars on its own.
There remains a strong need for ongoing screening for diabetes and heart disease, awareness, education, and lifestyle changes. Who oversees this? This was all discussed at the 3RD Annual Heart in Diabetes Conference in Philadelphia July 12-14, 2019. Since obesity, metabolic syndrome, and cardiovascular disease have no signs of remission, an exciting thought was put into place, proposing a new sub-specialty called cardiometabolic medicine. Many patients are still unfamiliar with metabolic syndrome and its implications.
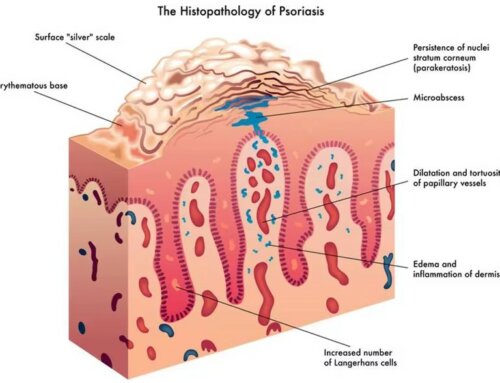
What Is the Metabolic Syndrome and What Can It Cause?
The metabolic syndrome is extremely common as a precursor to pre-diabetes and type 2 diabetes. It includes several criteria listed below. These numbers should be a wake-up call to your physician for future health problems including heart ailments. Here are the current indicators:
- Waist circumference- signals abdominal obesity and insulin resistance – over 35 inches in women, over 40 inches in men. Physicians rarely check waist circumference which requires a simple tape measure placed above the hips.
- Blood pressure- equal or above 130/85 mm/hg.
- HDLs- (good cholesterol) less than 40 mg/dl in men. Less than 50 mg/dl in women.
- Blood glucose- above 100mg/dl and below 126mg/dl – known as pre-diabetes/ indicates insulin resistance.
- Triglycerides- above 150mg/dl.
- Small particle size and hard texture of LDL particles. (bad cholesterol).
- Pro-inflammatory state- high levels of homocysteine in the blood, an inflammation marker.
- Pro-thrombic state- increased coagulation of blood leading to blood clots.
What Adds to the Metabolic Syndrome?
- Too much empty sugar as in refined sugar and high-fructose corn syrup. This can cause a fatty build-up in the liver leading to non-alcoholic fatty liver disease -NAFLD.
- Extra pounds- excess fat can also build up as fat around and inside the liver. The liver can scar, harden and develop cirrhosis; cirrhosis is excessive liver scarring which is not reversible and can make it difficult for the liver to function. It is life-threatening.
- Soda- Research shows, “a lot of soda can lead to a fatty liver or NAFLD on its own.”
- Trans-fats- Although, recently seen a lot less in foods, they are artificial fats put in some packaged and pre-made foods, “partially hydrogenated.” Donuts, baked goods and packaged snacks.
- Alcohol- Alcohol intake is an independent predictor of metabolic syndrome. The more the person drinks, the higher the risk. The frequency and intensity matter. Do not start drinking if you are not already drinking. If you drink alcohol, limit it to one drink, daily for men over 65 and women, two drinks daily for men under 65. Do not add sweet mixers, soda or fruit juice.
Metabolic syndrome also increases with age. Highest seen in Hispanics women with fatty liver disease and polycystic ovarian syndrome (PCOs). The Endocrine Society just came out with a powerful statement, “Health care providers should regularly screen adults, ages 40-75, for the first five metabolic risk factors(indicators) leading to the metabolic syndrome, type 2 diabetes and cardiovascular disease.” By checking these indicators more can be done to identify future health problems and prevent cases of type 2 diabetes and heart disease.
Is There Really a Need for a New Sub-specialty?
Due to an increase in worldwide aging, with a large predominance in sedentary lifestyles and obesity, who is the best physician to treat this growing population? Each of these maladies are extremely costly on their own and can severely change medical outcomes in a domino effect. Presently, patients move between their endocrinologists, internal medicine doctors as well as cardiologists. Some patients see two-three different cardiologists; non-invasive, invasive and an electrophysiologist. Each of these specialists treat different heart problems; a non-invasive cardiologist performs tests that require nothing being done internally.
Included could be EKGs, ECHOs and stress tests. An invasive cardiologist performs procedures such as cardiac catheterizations, angioplasties or TAVR procedures repairing heart valves. Tubes and catheters are temporarily placed inside the body. This requires either an in-patient overnight hospitalization or admittance to an out-patient facility. An electrophysiologist specializes in cardiac arrythmias such as atrial fibrillation, PACs or PVCs. Patients move back and forth among different specialists with really, “no ownership” and often have overlapping treatment or somehow miss something due to, “So many hands touching the same patient.” As more and more treatment options become available and there is more specialization, it is difficult for a physician to “know and treat everything.”
What Specifically Is Cardiometabolic Medicine?
The term cardiometabolic was born about fifteen years ago. Although still just a concept, the latest interest in cardio metabolic medicine would ultimately include extensive training in internal medicine, preventive and non-invasive cardiology as well as specific aspects of endocrinology, targeting diabetes. This new sub-specialty could become, “home” to the many complicated patients with cardiometabolic and cardiovascular disease.
What Would Cardiometabolic Medicine Focus On?
- Pre-diabetes/insulin resistance
- Obesity
- Metabolic syndrome
- Type 2 diabetes
- Lipid control
- Hypertension/high blood pressure
- Lifestyle- smoking, alcohol intake, exercise, nutrition, stress management, depression/anxiety
- Basic cardiovascular testing- EKGs, ECHOs, exercise stress testing, cardio-CT-scans, calcium scores and cardiac rehabilitation.
- Up to date and complete medication management- new and existing drug therapies.
Why the Sudden/Urgent Need Now?
Drug therapies in the world of cardiometabolic medicine has skyrocketed in the last few years. There used to be a small core of medications for management; they have recently tripled in choices for diabetes, lipids and heart medications. For example, patients need to be on statins for cholesterol, fibrates for triglycerides, ACE inhibitors, ARBs, calcium channel blockers, beta blockers and diuretics for blood pressure, anti-platelet drugs for coagulation/blood clotting problems- Eliquis, Pradaxa, also aspirin and a slew of new diabetes agents. Examples of new diabetes drugs that focus on cardiometabolic issues would include:
- GLP1 receptor agonists (glucagon-like peptide) These cause the pancreas to produce more insulin after you eat and help keep blood sugars in an acceptable range. GLP1s also slow gastric emptying, help you lose weight and make you less hungry. The added benefit is they protect your heart, good for lipids, weight loss, blood pressure, endothelial function and cardiac ischemia. Examples would be Bydureon, Byetta, Victoza, Trulicity, Tanzeum, Lyxumia and Ozempic. GLP-1s are injectable (not insulin) either taking daily or weekly, depending on the brand.
- SGLT-2 inhibitors (sodium-glucose co transporter 2 inhibitors) These are pills, given for diabetes, specific to help reduce blood sugars by pulling sugar out thru the urine. Examples are Invokana, Jardiance and Farxiga. They are now considered cardiometabolic drugs too, since they reduce the risk of heart failure, lower glucose numbers and show good benefits against cardiac mortality.
Which MD Will Be the One to Watch for All the Complications?
When you treat the patient there are many things to look for based on medications alone. With everyone on board to treat, who is ultimately responsible? Do cardiologists know what to look for in diabetes, do endocrinologists know what to look for in heart disease? Can the internist handle all the above? When on a slew of medications for different ailments, who will ultimately be in charge of looking for:
- Extremely high or low blood sugars due to diabetes pills and insulin.
- Bleeding problems from anti-platelet drugs.
- Lightheaded/dizziness from vasodilators.
- Need for extra potassium or magnesium. Need for less potassium depending on the heart medication.
- Noting stomach issues such as nausea and vomiting from GLP1s or DPP4s.
- Developing pancreatitis from GLP1s.
- Genital and urinary tract infections or acute kidney injury from SGLT-2s.
- Muscle cramps and pains from statins.
- Coughs associated with ace-inhibitors.
- Diabetic ketoacidosis from SGLT2s or lack of insulin.
- Sudden bleeds from anti-platelet drugs.
- Rare, but risks of gangrene from SGLT2s.
- Bone fractures, low bone density from SGLT2s.
What Could the Possible Training Include?
Until recently, there was no specialty for the elderly, but when a need developed, the field of gerontology or geriatrics was born and introduced. “end of life care and pain management” established palliative medicine as well. Since this field is relatively new to discussion, there is no specific plan yet in place. Some physicians including preventive cardiologists think they already do a complete job of treating these medical issues. At this point, an involved physician from the University of Colorado named, Dr. Robert Eckel has made certain suggestions. He is an internist/endocrinologist who specializes in metabolism and metabolic disease. Dr. Eckel is also well versed in nutrition and cardiac disease seen in diabetes.
According to Dr. Eckel, “It could include two years of internal medicine and four years of metabolic/cv prevention. “The metabolic component would include areas of diabetes, type1/2, metabolic syndrome, lipids, genetics and lifestyle. There would be no endocrine focus on thyroid, adrenal, pituitary, bone or reproductive medicine as seen in a traditional endocrine specialty. There would be no cardiac procedure training, but inpatient and non-invasive cardiology would be included. Also, not given would be critical care section. This specialty would bolster up lifestyle and nutritional training, since no medical specialty, presently covers them.
Benefits and Negatives
The benefits would be to handle a current large population and growing group who requires specific and complete care. The training would help pave the way for both physicians and patients with these specific and common problems. The negatives are that not all sub-specialties are on board. There could be, “turf wars” among different specialists who claim rights to the patients.
According to the senior VP of The Board of Internal Medicine, Dr. Furman S. McDonald, “The theoretical demand is not enough to be recognized as a sub-specialty.” Some think it overlaps preventive cardiology and that specialty should fine tune their skills for this population. No final decisions have been made. If it happens, it could take 10-20 years to get the plan in place. Creating a defined, developed training program that has a well-placed curriculum is a must. Then a class must go thru the entire program to get to the final stage of treating patients.
Who Will Be Involved If the Process Eventually Does Occur?
- American College of Cardiology.
- Obesity Society.
- American Diabetes Association.
- Academy of Nutrition and Dietetics.
- American College of Preventative Cardiology.
- National Lipid Association.
- American Board of Internal Medicine.
- Endocrine Society.
- American Heart Association.
- Cardiometabolic Health Congress.
- American Association of Endocrinologists.
Medicine is always evolving with better treatment, procedures, technology and care. The future can make things more complicated or not, depending on how we see and do what needs to be done. Be your own advocate. Follow along so you can be aware of the possible changes in medicine, in the future.





Leave A Comment