Diabetes and Psoriasis – What is the Connection?
“Diabetes increases the likelihood of developing psoriasis, a condition that causes red, itchy, raised patches of dry skin.” There are 125 million people worldwide with psoriasis and 3% of Americans have psoriasis. People with diabetes are at a higher risk for multiple skin disorders, not just psoriasis.
Diabetes and psoriasis are chronic yet distinct conditions. Both are associated with systemic inflammation and a higher risk of heart disease. Both are associated with an increased chance of skin infections which may lead to secondary infections and higher blood sugars. People who have psoriasis are also more likely to develop type 2 diabetes.
Generally, the more severe the psoriasis, the greater the chance of getting diabetes. Diabetes is 1/3 higher in those with psoriasis compared to those without it. Neither disease is contagious so it can’t be spread through touch or contact. There are 8 million Americans that have psoriasis and there are over 34 million Americans with diabetes.
The metabolic syndrome is also seen in both these diseases. The metabolic syndrome includes a large waist circumference, hypertension, high cholesterol, obesity and elevated triglycerides. People with psoriasis may be at higher risk for basal cell cancer, squamous cell cancer and lymphoma. If you have diabetes, you are also at a higher risk for cancer.
What is Psoriasis?
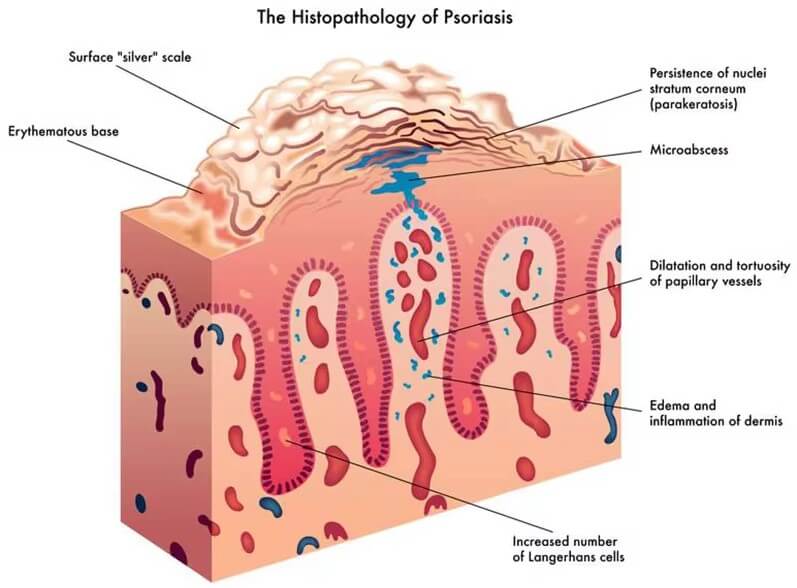
Psoriasis is an autoimmune disease. This means it is triggered because of an abnormal immune system response. Your immune system helps protect you against viruses and bacteria. It defends the cells of your body. The immune system is a network composed of organs, cells and proteins. White blood cells, called T cells, mistakenly attack skin cells and skin cell production piles up instead of shedding.
Psoriasis is seen more frequently in both adults and children with type 2 diabetes. One theory is that “psoriasis could change the use of the immune system leading to the killing of beta cells in the pancreas that make insulin.” Some scientists believe the connection may have to do with the obesity epidemic that is commonly seen in adults and children. Both diseases are systemic and are involved in insulin resistance.
What about inflammation? Inflammation is a process that can be both good and bad for your body. It can signal the body’s response to an illness, germs or injury. The good is part of the healing process. The bad is that it could cause pain, swelling, redness, heat and drainage.
Inflammation in psoriasis leads to insulin resistance. This inflammatory process causes the liver to produce more sugar and the pancreas to make less insulin.
How is Psoriasis documented?
Your physician can inform you if you have a mild, moderate or severe case of psoriasis. This depends on how much of your “overall body surface is affected.” A mild case covers 1-3% of your body, a moderate case covers 3-10% of your body, and a severe case covers over 10% of your body.
What are common causes of Psoriasis?
The actual cause of psoriasis remains unknown but there are certain factors involved. It can come on quickly or slowly. It often appears at ages 15-35 or 50-60 but can occur at any age. There is no cure, as with diabetes, but it can be managed. Usually, the body process of skin cell turnover takes 3-4 weeks. With psoriasis, the process takes 3-7 days because of the rapid turnover of skin “the skin cells are not fully developed and build up on the surface of the skin.” Psoriasis presents as flaky, itchy, crusty, red and scaly, silver patches.
Genes. As in diabetes, psoriasis runs in families. If you have a family member with it, your chances will increase but it does not mean you will get it too. You may inherit one or more genes that affect your immune system making you more prone to it.
Existing health issues. If you have ankylosing spondylitis, diabetes or rheumatoid arthritis, your chances for getting psoriasis increase.
Changes in hormones. During puberty, pregnancy and menopause, hormone levels fluctuate and may result in developing psoriasis.
Koebner Phenomenon (KP). “The Koebner Phenomenon was first described by Heinrich Koebner in 1876. It is the appearance of new skin lesions on previously unaffected skin secondary to trauma.” Common skin injuries such as a scrape, insect bite, sunburn or a gash can initiate psoriasis if the tendency is already present. Surgical scars, tattoos and piercings can also be affected as well as jewelry rubbing on your skin or your shoe/sock rubbing on your feet. A new psoriasis lesion can appear based on the trauma to your skin.
What are some triggers for Psoriasis flare ups?
You may experience remission from your psoriasis between 1-12 months. Sometimes the remission lasts even longer. That said, there are common triggers which may set off an episode. They can include:
- Environmental influences. Air pollution from wildfires, automobiles and factories.
- Infections. Having a respiratory infection, staph or strep. An ear infection, bronchitis or tonsillitis can trigger it. A bacterial or viral infection may be a trigger.
- Vaccines. The flu, pneumonia and yellow fever vaccines have triggered episodes of psoriasis. Covid vaccines can be a trigger, too.
- Stress. A life changing event like a divorce, a wedding, a new birth, a new job, purchasing a new home, a death, and even a hectic time of life (either good or bad), could all become triggers for a flare-up of psoriasis.
- Weather. Cold and dry weather. Low levels of sunlight and humidity can be a trigger. Winter season is more of a trigger for psoriasis than summer weather.
- Sunlight. Too much direct sunlight may be a trigger.
- Air-conditioning. A room that is too cold from AC or constant exposure to blowing AC can be a trigger.
- Medications. Certain medications can be triggers for psoriasis. Blood pressure medications including beta blockers or ACE-inhibitors. Lithium which is used for bipolar disorder. NSAIDS-Ibuprofen, Advil, Aleve used for a fever or inflammation. See if you can take Tylenol instead. Anxiety medications such as Xanax, Valium and Klonopin can be a trigger.
- Skin injuries. Even shaving injuries to your skin may trigger an episode of psoriasis.
- Diet influences. Eating red meat, full-fat dairy, processed or ultra processed foods, sodium, refined sugar and drinking alcohol can trigger an episode. “There is a well-documented relationship of eating too much sugar, inflammation and psoriasis.” Psoriasis medication treatments work better with less side-effects when you do not drink alcoholic beverages or eat processed foods. Spicy and hot foods such as hot sauce, chili pepper or paprika can trigger an episode.
- Weight. Weight gain could influence your health and diabetes as it raises your blood sugars. Weight gain can also influence your skin. Psoriasis gets worse with weight gain since skin becomes itchy. Excess skin creates skin folds, more perspiration, and making it uncomfortable and more difficult to exercise. This leads to more weight gain and higher blood sugars and more psoriasis outbreaks.
- Smoking cigarettes. Either smoking or breathing second or third hand smoke is a trigger.
- Gluten. People with psoriasis are more prone to celiac disease which is an “autoimmune sensitivity to gluten” and food products with gluten.
What is gluten?
Gluten is the general name for the proteins found in wheat, rye and barley. “Gluten is responsible for the elastic nature of dough and its chewy texture.” Oats do not contain gluten, but they are often grown near, processed and transported with wheat, barley and rye. These oats may cause a gluten reaction. Bread, cereals, pasta, baked goods, soups, salad dressings, granola bars, beer, food coloring, and commercially prepared sauces contain gluten.
Try to keep track of the triggers that affect you and your psoriasis flare-ups. Keep them to a minimum for less skin outbreaks.
How is Psoriasis diagnosed?
- Physical exam. Checking the entire body including skin folds and genitals. Check the scalp, nails and nailbeds. Ask and check for joint swelling and joint pain. Look at knees and elbows.
- History. A complete medical history must be taken.
- Biopsy. A skin biopsy can distinguish between other skin ailments/diseases and psoriasis.
- Blood tests. Included may be ANA, CRP, ESR, RF, and an anti CCP. These blood tests indicate inflammation in the body. Your health care provider will recommend specific blood tests and give you a written prescription.
Who should be part of your medical team when you have Psoriasis?
- Endocrinologist. If you also have diabetes
- Internist or PCP. The “captain of your ship” to coordinate all your medical care
- Dermatologist. Specializes in skin disorders, rashes and skin cancer
- Rheumatologist. Specializes in psoriatic arthritis and joint problems which are common with psoriasis
- Dietitian. Specializes in creating a healthful eating plan with you. Both diabetes and psoriasis can benefit from a Mediterranean diet.
- Pharmacist. Understands and can explain all the medications needed for psoriasis, diabetes and any other disease process you may have. Always ask about drug interactions when starting a new medication.
What are the different types of Psoriasis?
- Plaque psoriasis. 80-90% of psoriasis cases are plaque psoriasis. There is a buildup of skin cells that are red, flaky, itchy and sore with white or silvery scales. The red color comes from the increased blood flow to the specific area. The plaques can be thin or thick. They can be found on the trunk of the body, face, palms, feet, elbows, knees, armpits, joints, soles of the feet, groin or buttocks. It is not sexually transmitted. It is not transmitted by touch.
- Scalp psoriasis. The plaques can also appear on the scalp. This is different than dandruff. Dandruff is white flakes with a tight scalp. Scalp psoriasis are well-defined red, scaly patches.
- Pustular psoriasis. Usually seen on your palms or your soles. Presents as generalized very dark red patches covered with small pustules. It can crack and hurt and is more often seen in women who have diabetes. This type is extremely painful.
- Nail psoriasis. Seen on finger or toenails, may come or go over time. There is pitting, ridge formation, denting, a change in color of the nail to yellow or brown, a change is nail shape, thickening of the nails and lifting of the sides of the nails.
- Guttate psoriasis. This is most common in children after they have had an infection especially strep throat. “Tear drop patches appear.”
- Inverse psoriasis. Located in the skin folds, groin, under the arms, under the breasts and in the buttocks. They appear as mostly red patches with no or few silver scales. Plaques are more moist than dry.
- Psoriatic arthritis. Affects the joints, skin and nails. Joints can be swollen and painful. The tendons and ligaments are also affected. It may cause irreversible joint damage. It is a type of “inflammatory arthritis.”40% of patients with psoriasis develop psoriatic arthritis.
- Erythrodermic psoriasis. This is a rare form but can be life-threatening. It is seen more commonly in men. The heart rate goes up along with body temperature. There is intense swelling, itching, and pain. It can stay away for months or years and then suddenly reappear.
- Psoriasis usually appears on both sides of the body. For instance, if one knee or elbow has it, then usually the other one has it, too.
What are common treatments for Psoriasis?
- When you also have diabetes, you are often started on a GLP-1 medication injection, such as Ozempic or Mounjaro. These medications have an impact on weight loss and can positively impact both medical conditions. Blood sugars go down, appetite is suppressed, the immune system slows down and inflammation is eased in the entire body. Usually, your PCP or endocrinologist will put you on this.
- Lotions, sprays, ointments and emollients should be used as per your health care professional’s direction. Topical treatments are usually “1st line treatment since it does not treat the underlying systemic inflammation. For the more exposed areas of your body like hands, fingers and face, the more times these products should be used. These products should be applied prior to swimming, walking outside and gardening as a “protectant.” Sometimes cold-water compresses are used prior to lotions, sprays, creams and emollients. Topical treatments often have various complaints from patients. Topical psoriasis treatments are considered “messy, odorous, staining on clothes, visible, time consuming to put on and highly irritating in the genital areas.”
- Lotions and sprays. Lotions are thin, spread easily but are not very moisturizing. Sprays absorb quickly, are easy to use, and are especially good for harder to reach areas and can cover infected areas that should not be touched.
- Mild topical creams. Creams absorb quickly, are not too greasy and are best for day use. These creams are started early, and they may take 6 weeks or more to see a change in your skin texture. In 2022, new non-steroidal creams were FDA approved and introduced to the market. Tapinarof cream is a relatively new prescription cream used for plaque psoriasis, but it may produce “multiple side-effects.”
- Topical steroid creams. “Since plaque psoriasis is not curable, steroid creams are a poor choice. They should only be used short term.” The side-effects become too great. Topical steroids dangerously thin out the skin. Steroids also raise blood sugars which is a negative effect especially for those with diabetes.
- Ointments are more greasy but stay on the skin better and longer than creams. Ointments work best when skin is very dry with thick, big patches of plaque. They work well at night since they are extremely moisturizing. Ointments are usually free from preservatives and good for highly sensitive skin. They should not be used on open infected weeping areas. They may be more expensive.
- Emollients moisturize skin and lower itching and scaling. They can be a prescription or an OTC emollient. Emollients can be transferred to small pods and tubes for easier transport. They are applied to the skin for soothing and hydration. Emollients should be smoothed into skin and not vigorously rubbed into skin which can further irritate it. Emollients should be placed on skin in the same direction as hair grows so you do not block the hair follicles. It is difficult to over-use emollients. The protective film layer traps moisture into the skin.
- Emollient soap substitutes. Sometimes regular soap is too drying and damaging to skin. With psoriasis, an emollient soap substitute should be used instead. If your skin burns, turns red or overheats from regular kinds of soap and cleansers, talk to your physician about emollient soap substitutes. They do not feel like regular soaps but are good for cleansing your skin.
- Special shampoos are used for scalp psoriasis. There are OTC shampoos that contain tar and salicylic acid. Other shampoos contain retinoids and vitamin D creams. They are different than shampoos for regular dandruff.
- Phototherapy. This involves use of light therapy used directly on the patches. Phototherapy is not prescribed to patients who also have skin cancer. It uses natural and artificial light and is not the same as a tanning bed. Light therapy is usually given in a hospital, out-patient center or in a physician’s office with a dermatologist supervising the procedure. There is Ultraviolet B (UVB) phototherapy. “The wavelength of light slows skin cell production.” It is usually done for 6-8 weeks, 2-5 times a week for a few minutes per session. The light intensity, duration of light therapy, and the total number of treatments vary per person. Combination light therapy includes light therapy along with lotions, creams, ointments or emollients. Other light therapies include narrowband UVB therapy, PUVA therapy and excimer laser light therapy.
What other treatments are currently used for Psoriasis?
When symptoms become moderate or severe, therapy usually switches to a prescription pill or injection/infusion. Always talk to your health care provider for all your best options. Moderate to severe symptoms range from painful, large areas, burning, stinging, tightness, itching, tenderness, cracking, bleeding and oozing.
The psoriasis generally covers 10% or more of the body. These medications may make it more difficult for your body to fight off serious systemic infections.
- Systemic. oral or injected medications that work on the entire body. These medications can lower the immune systems response and general inflammation.
- Older systemic medications. This includes Cyclosporine and Methotrexate. They calm the immune system and slow skin cell production. These medications were used “as cancer drugs and as transplant rejection drugs.” They can raise blood pressure and cholesterol levels. They are both extremely strong and toxic.” They come with many side-effects and may damage both the kidneys and liver function. People with diabetes are at an already higher risk of kidney disease.
- Acitretin. An older pill which is an oral retinoid. It reduces skin cell production but has multiple side-effects. Acitretin can raise cholesterol levels, which are usually higher when you have diabetes.
- Newer pills. This includes Otezla, Sotyktu and Tremfya.
- There are now 13 FDA biologics FDA approved. Biologics are made from living cells. These are injections/infusions for moderate to severe plaque psoriasis. Most people can self-inject at home. You can also receive them as an infusion at your doctor’s office. Included would be Enbrel, Remicade, Skyrizi, Cimzia, Taltz, Cosntyx, Humira, Stelara and Bimzelx.
Natural ways to help control Psoriasis
Always consult your physician and never stop taking your prescription medications. You may want to “add on” some of these suggestions which are considered more natural. Consult with your medical team before trying any of them. About “51% of people with psoriasis use some type of complementary treatment besides medication.”
- Acupuncture. Acupuncture is an ancient practice of inserting thin needles into the skin. It’s been around for thousands of years. Although there are no confirmed studies between psoriasis and acupuncture, there are little risks. It is worth a try as adjunct therapy. Some people get relief from the itching and burning.
- Daily baths. Short, tepid, warm baths and patting skin dry is a relief for many patients. Never use hot water as it is too irritating to your skin. Colloidal oatmeal baths or paste may also soothe skin. Put oatmeal in a food processor and grind. Add a bit of water to make an oatmeal paste. You can also purchase Aveeno OTC colloidal oatmeal bath products. Using a good moisturizer or even Vaseline or Aquaphor after a bath can be comforting to your skin.
- Cold packs. “Cold confuses the brain since you can’t feel cold and itchy at the same time.” Cold therapy also helps with joint swelling. Use for 10-20 minutes and do not place cold pack directly on your skin. Place a wash rag between your skin and the ice pack.
- Capsaicin. Found in chili peppers, you can eat them or use in an OTC gel to help joint pain and relieve swelling.
- Apple cider vinegar. Made from fermented apple juice, a tablespoon of apple cider vinegar can be diluted in water and used for an itchy scalp. Do not use on open wounds, cracked or split areas. Put on scalp, let it dry and rinse off with cool water.
- Vitamin D supplements. Never take without consulting your health care provider. Consider 600-800mg a day in a liquid, gel or capsule supplement. Vitamin D is fat soluble, and it is possible to take too much.
- Biotin. A supplement that helps regulate skin cell signals. Consider taking 30mcg daily.
- Omega 3 fatty acids. Taken as a capsule supplement, research shows it “does improve itching, redness and inflammation.” Omega 3s are found in nuts, seeds and fatty fish such as salmon or herring.
- Methylsulfonylmethane (MSM). An anti-inflammatory supplement especially good for your joints. More research is needed but 2000-4000 grams a day is often used. It is OTC.
- Turmeric. The curcumin found in turmeric decreases inflammation which may help patches and lesions with few side-effects. There is a turmeric spice powder which can be added to drinks and poured onto foods or turmeric tablets.
- Probiotics. More research is needed but research points to having less systemic inflammation when you take a probiotic.
- Folic Acid. People with psoriasis usually have low levels of folic acid and high levels of CRP (a body inflammation indicator). Folic acid is a B vitamin.
- Selenium. It is an essential trace element that helps decrease inflammation in the body. 55mcg a day is recommended.
- Vitamin A. Both topical and oral administration may be helpful. Good results have been seen with 700-900mcg a day. It is naturally found in orange and yellow vegetables like yellow peppers and carrots as well as egg yolks, spinach, avocados and kale.
- Glutathione. Levels tend to be low when you have psoriasis. Glutathione boosts the immune system. It is found in garlic, onions, broccoli, cabbage and cauliflower.
- Aloe Vera. Aloe Vera is found naturally in this succulent plant. Break off a piece of the plant and remove the gel or OTC gel can be used to help relieve pain, redness and scaling. Keep in the refrigerator for a cooling affect.
- Coconut oil/olive oil. Used as a natural skin moisturizer.
- Cotton or Bamboo towels and sheets. They are gentler on your skin.
- Elimination diet. Depending on how you feel and the symptoms of your psoriasis, you may consider trying the elimination diet. Do consult a dietitian or other health care provider if you decide to try it as it is difficult to follow. Many times, people may attempt to eliminate gluten, dairy, caffeine, sugar, grains, artificial sweeteners, alcohol and processed foods from their diet. Eventually you may reintroduce some or all these foods slowly back into your diet depending on psoriasis symptoms and what your health care provider decides.
Finally
Never run out of any of your medications or supplies whether it be for your diabetes or psoriasis. Get 5 minutes of sunshine a day which can help improve your skin conditions. Do not over-do it. Always wear sunscreen with at least 30 SPF that is fragrance-free, broad spectrum and for sensitive skin.
Use a sunscreen lotion or cream instead of a spray. Find shade, wear a wide-brimmed hat and sunglasses. Carry an umbrella for sun protection. Stay cool if possible. Take breaks from the heat and outdoors. Heat and excessive sweating can trigger symptoms of psoriasis. Never scrub your skin when you are washing or drying your skin. Gently wash and tap dry.
Use a humidifier in your home to increase the moisture level. Dress in soft layers to keep skin protected from hot or cold temperatures. Avoid smoking and too much alcohol. Consider joining a support group in person or on Zoom for your condition.
Remain active with your exercise but do not get over-heated. Always ask questions when you are at your health care provider. Both diabetes and psoriasis are treatable and manageable diseases.
Remember, heart disease, diabetes, metabolic syndrome, non-alcoholic-fatty-liver-disease and psoriasis are all linked to systemic inflammation. Find out your diagnosis and then treat the ailment with the best specific treatment for you.
References:
- https://www.webmd.com/skin-problems-and-treatments/psoriasis/cm/psoriasis-treatment-with-other-conditions
- https://www.ncbi.nlm.nih.gov/books/NBK553108/
- https://diatribe.org/understanding-diabetes/psoriasis-and-diabetes-whats-connection
- https://www.nhs.uk/conditions/psoriasis/
- https://www.nhs.uk/conditions/emollients/
- https://www.webmd.com/skin-problems-and-treatments/psoriasis/diabetes-psoriasis
- https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2021.605691/full
- https://www.bezzypsoriasis.com/discover/pso-living-well/health-ask-the-dietitian-what-should-i-know-about-sugar-and-psoriasis/
- https://www.goodrx.com/conditions/plaque-psoriasis/psoriasis-and-diabetes
- https://www.medicalnewstoday.com/articles/52457
- https://www.health.harvard.edu/diseases-and-conditions/a-deeper-look-at-psoriasis
- https://www.forbes.com/health/conditions/psoriasis/
- https://www.verywellhealth.com/psoriasis-7099867
- https://www.medicalnewstoday.com/articles/325378?utm-source
- https://www.webmd.com/skin-problems-and-treatments/psoriasis/cm/drugs-trigger-psoriasis-flares
- https://celiac.org/gluten-free-living/what-is-gluten/






Leave A Comment