Medical Equipment Does Matter!
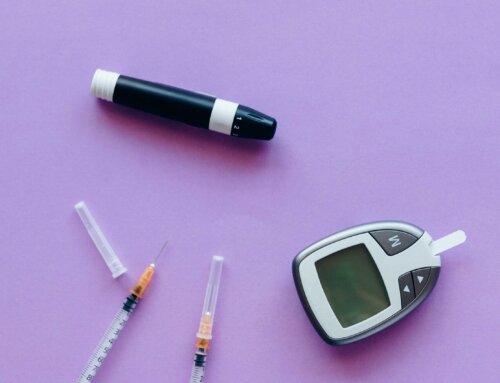
People with diabetes depend on certain medical equipment to help them maintain the best possible blood glucose control and over all health. From determining their blood glucose levels to checking their blood pressure, people need equipment for proper diabetes management. Find out why medical equipment does matter when it comes to optimum health with diabetes.
Size Matters When It Comes to a Blood Pressure Cuff
People with diabetes are prone to high blood pressure, cardiovascular disease, and other heart-related problems. It is important to keep track of your blood pressure at home in between medical exams. Size matters when it comes to choosing a blood pressure cuff. If it is too small or too large, a person can get inaccurate blood pressure readings. Poorly fitting cuffs will not give an accurate blood pressure reading.
Choosing and Using a Blood Pressure Cuff
The two basic types of blood pressure cuffs are used on the wrist or upper arm. Usually wrist monitors are one-size-fits-all. The strap can be adjusted from about 5 inches to 10 inches to accommodate wrists of all sizes. Wrist cuff monitors are not as accurate as arm cuff monitors. Upper arm monitors vary in cuff sizes and it helps to measure your upper arm when seeking the best fit. Use a measuring tape at the exact center point between the elbow and shoulder. Sizes range from small to extra large. When the cuff is too small the blood flow is restricted and can lead to a false high blood pressure reading. Conversely, if the cuff is larger than the circumference of your arm, the blood flow is not restricted enough which can lead to an inaccurately low blood pressure reading. The cuff should be properly positioned by your brachial artery. The air tube should be centered on the arm with about a 1/2 inch of free space from the elbow. Wide-range cuffs are available for people with larger arms. Make sure your arm is at 90 degrees when measuring blood pressure for the most accurate result.
Basics about Blood Glucose Meters

Finding the Right Blood Glucose Meter
When it comes to expenses, factor in the cost of the blood glucose strips that must be used with that specific meter. This can add up for someone who monitors his or her blood glucose several times a day and is paying out of pocket. Contact your insurance company to find out which meters and strips are on the preferred list to minimize your out-of-pocket expenses. If you do not have health insurance, try to find an online diabetes supply company that offers discounted prices. Accuracy is another factor to consider and discuss with your doctor. The Food and Drug Administration (FDA) current standards require 95 percent of all meter test results to fall within 20 percent of the lab results for your blood glucose level which are greater than 75 mg/dl. For values below 75 mg/dl, it is within 15 mg/dl. For example, if your blood glucose is 100 mg/dl, the meter could read anywhere from 80 and 120 mg/dl to be considered accurate. Most meters are fast and will display your testing results in less than five seconds. When it comes to size and shape, personal preference is the key consideration. People who have visual problems may want a large meter that makes it easier to see the screen and buttons. There are also talking meters that do not require reading the printed number. Those who are on-the-go might prefer a smaller, more compact meter. A backlight, color and/or high contrast can also be helpful for people who have difficulty seeing the results on the meter.
Meters That Talk to People with Diabetes
A talking blood glucose meter can be a major help for people with moderate to permanent visual impairment. For those who cannot see a large-print screen, a talking meter can convey essential results to help them successfully check their blood glucose levels.
Considerations When Choosing a Talking Meter
A talking meter should be a convenient size for a user who needs to carry it in a pocket or handbag. The voice should be clear enough so the user can hear it. The language should be understandable for the user, such as English or Spanish. The voice should guide the user through the steps for checking blood glucose. Consider if the volume is adjustable and whether an earphone can be used when you are checking your blood sugar in public. The ends of the strips should be simple to identify and the strips should be easy to insert with minimal vision. Other considerations are whether test results can be repeated and stored.
Getting a Blood Sample for the Meter

Alternate Site Testing
Constantly taking blood from the fingertips may lead to soreness. This is particularly noticeable for people who use their fingertips to type and perform other routine tasks. The sides of the finger have better blood flow and fewer nerve endings. Change the finger you use for testing regularly to avoid soreness in one finger. Avoid the thumb since it is used for most daily tasks. The majority of meters also allow for alternative site testing. Blood can be drawn from less painful areas such as the forearm or palm of the hand. Users must also remember it takes around 20 minutes for alternative site measurements to show changes in your blood glucose levels. If you suffer from hypoglycemia often, continue to use your fingertips to prevent severe problems.
Blood Glucose Meters with a Download Feature Can Be Helpful
Many meters will store blood glucose readings and offer the ability to upload pertinent data to a PC or smartphone. This can help users to determine trends and better manage their diabetes. These results can also be shared with your health care team to help spot patterns.
Downloading Data in a High Tech World
Consider the ways data can be downloaded from a blood glucose meter. Some use a USB port that plugs into a computer. Others have Bluetooth technology so the data can be downloaded to a computer without using wires. There are also meters that are mobile-app friendly. This makes it possible to view the data from a smart phone. The need for storage is based on how frequently you check your blood glucose levels and the frequency of downloading and reviewing the data. For example, your health care provider might want to view 30 or 60 days of results. Consider the number of glucose records that must be stored to share this data with your doctor.
Using a Control Solution
A control solution is used to check your meter and test strips accuracy. This is an important step to remember. Using control solution can provide essential peace of mind that your meter and test strips are performing as they should for the best possible diabetes management.
How to use Control Solution
The FDA provides suggestions for using control solutions. It should be used whenever a new container of test strips is opened. If you drop the meter, use control solution to check its accuracy and confirm it is still able to report testing results quickly. If the results are unusually high or low, use control solution to verify the meter is working properly. Control solution is perishable and often viewed as an added expense. However, an opened vial should always be discarded after 90 days. Throw away expired control solution, even if it has never been opened. Sometimes this cost can be minimized or eliminated by asking your doctor to write a prescription for control solution as it is covered by certain types of insurance or Medicare B.
Consider the Quality of Test Strips
While they may appear to be basic strips of plastic, test strips are actually medical equipment that represents the science, technology, and engineering used to help people manage diabetes. First used for home testing in the 1980s, test strips have evolved over the past few decades to use less blood and deliver greater accuracy in less time. Today glucose is converted into an electrical current that goes through the strip and gets read by the meter.
Selecting Test Strips
As mentioned above, the measurements for a home meter need to be within 20 percent of the lab-tested value. The FDA is working on making these standards more stringent. Test strips play a major role. They should not be exposed to temperature extremes, artificial light or humidity to avoid compromising the enzymes in the strips. They should be kept in the vial until used. Test-strip codes enable the meter to detect information from the test strip. Some meters require the use of a code chip or manual entry of the code. Automatic reading is easier and may be more accurate. Expired strips will also cause an error. Insurance plans cover specific test strips which is a major factor in which ones to choose.
People with diabetes need home medical equipment to help monitor their condition. Accuracy, ease of use, and cost are major factors to consider when choosing this equipment. The right equipment can help you detect important changes, avoid health emergencies, and achieve maximum well-being.






Leave A Comment