Diabetes is a chronic health condition that requires constant management. Taking care of yourself is essential to feel your best at all times. Find out what kind of diabetes patient you are and ways to improve your self-management routine.
Do You Keep Your Medical Appointments?
It is important to work with a dedicated health care team to properly manage diabetes. Scheduling and keeping all your medical appointments is essential for optimum health.
A Doctor Checklist
Diabetes can be linked with a variety of other health conditions including vision problems, dental decay, obesity, high blood pressure, heart attack, stroke, skin disorders, foot problems and neurological concerns. Talk to your primary care physician about the list of doctors you should consult with. Your primary physician is the “ships captain” and they should be coordinating all your care. This may include an ophthalmologist, dentist, cardiologist, endocrinologist, dermatologist, nutritionist, diabetes nurse educator, neurologist and podiatrist. Each doctor will establish a check-up schedule to help you maintain the best possible health. Make sure to keep these appointments to avoid more serious health complications. Create a checklist so you don’t forget any checkups. Keep a calendar with appointment cards to confirm all visits. Make sure your primary care physician is receiving all reports from the other physicians to maintain a complete record. This will cut down on confusion as to each physician’s separate responsibility.
Do You Take Medications Correctly?
Each diabetes patient has a different management plan including medications. Most patients require the administration of certain medications, such as pills, injectables or insulin. Taking your medications correctly and on-time is essential to maintain healthy blood sugar levels. Failing to take medications as directed can lead to health problems and possible emergency situations. Never run out of your medication and always refill when you have a week’s worth of medication available.
Maintain a Log
Maintain a log to verify you are taking all medications on schedule. Have your primary doctor print out a list of all your medications, the dosages, and the time to take them. This is useful in an emergency and should always be with you. It can also be stored on a Smartphone, linked to your ICE (in case of emergency) contact number(s). Place a list on your refrigerator to help EMTs when an emergency occurs. Wear a medical necklace or bracelet listing your medical problems in case you require emergency care and are unable to speak. Consider a medical alert service especially if you live alone. If you are traveling, moving, or have a change in schedule, consult with your doctor to update your medication schedule. Always store your medications at the right temperature to ensure they are effective. Never leave medications including insulin in extreme heat or cold and never store or leave them in the car. Talk to your health care team about coordinating your meal and medication times. Taking medications at the wrong time will not allow them to be as effective.
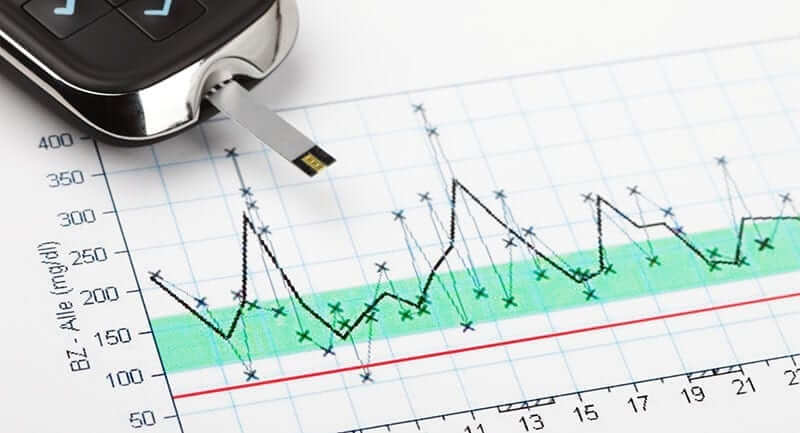
Do You Know Your Numbers?
People with diabetes should be aware of their important numbers. This includes blood sugar levels, blood pressure, A1C, cholesterol level, triglyceride levels, BMI and weight.
Find Out the Facts
Talk to your doctor about ongoing testing to determine your numbers and how they will adjust your diabetes management plan. Your goals are to stabilize your blood sugar levels, have a normal blood pressure level, and maintain a healthy weight. If your numbers get out of line, consult with your doctor to find out how to get back on track. Do not wait for the next appointment which may be 3 months away if you see large swings in your numbers.
Do You Test Your Blood Sugars?

Blood Sugar Testing Tips
Always have plenty of diabetes supplies on-hand at home, at school, and at work to test your blood sugars. Be aware of the times when your blood sugar levels can fluctuate, such as before and after meals, during stress and exercise. Keep glucose tablets handy in case your blood sugar levels plummet. Be aware of what to do if you experience hyperglycemia or hypoglycemia. Maintain a record of your blood sugar test results to share with your physician during routine exams. You can use a simple log book or download your readings on a spreadsheet. Many physician offices now have the capacity to download your numbers at the office. This helps determine certain patterns and whether your medications and management plan need to be adjusted.
Do You Test Your Blood Pressure?
Being aware of your blood pressure helps you be proactive about your heart health. Purchase a home blood pressure device to help you stay on top of your numbers. Chart them along with your blood sugars. If you choose not to test blood pressures at home then consider stopping at the pharmacy or grocery store for a reading. You may notice completely different readings between the physician’s office and your own readings. This could be due to “white coat syndrome” which is often experienced in the doctor’s office and could show unusually high, inaccurate numbers.
Do You Make Time for Exercise?
Regular exercise can help people with diabetes live longer, healthier lives. It is a way to get in shape, maintain a healthy weight, and reduce stress. Most important, it reduces insulin resistance which is the basis of diabetes type 2. Even if you have a hectic schedule, it is essential to make time to exercise.
Get Moving Every Day
The goal is to get moving for at least a half hour every day. This includes stretching, strength training, and aerobic activities. Walking, biking, swimming, and sports are all ways to add aerobic activity to your day. Resistance bands and weights are good for building stronger muscles. Stretching may include simple toe touches and arm circles as well as exercises such as Tai chi and yoga. Having a workout machine at home can make it easier to fit exercise into busy days or during inclement weather. Consider a treadmill or a stationary bike. Fit movement into each day by taking the stairs rather than the elevator and parking further away from your destinations. Take a walk at work during your lunch break. Commit to walking the dog every night to include more movement in your day. Stand and move.
Do You Take Care of Your Feet?
People with diabetes are prone to developing neuropathy and may not feel injuries to their feet. These injuries can lead to serious health issues. Taking care of your feet is important to avoid health complications.
How to Take Care of Your Feet?
Always remove your shoes during routine medical exams so the doctor can check your feet. Examine your feet daily for sores, cuts, and other irregularities. Use a mirror if you have trouble seeing your feet. Report issues to your doctor immediately. Wash your feet daily with warm water and mild soap. Dry them gently and completely with a soft towel. Apply diabetes foot cream to your feet, avoiding the areas between your toes. Trim your toenails straight across if you can. Consult a podiatrist if you have any ingrown toenails or other toenail deformities. Calluses can be gently minimized by using pumice. Never cut or shave calluses. Find out if your insurance will cover pedicures from a podiatrist. Have your feet measured to ensure you wear shoes that fit properly. Wear diabetic socks with no seams to avoid abrasions. Flat, wide toe-box, comfortable shoes are the best choice. Stay away from open shoes, such as flip-flops, and never go barefoot. Wear slippers at home and water shoes at the beach or pool.
Do You Take Care of Your Eyes?
People with diabetes are prone to certain eye diseases, such as cataract, glaucoma, diabetic retinopathy, and diabetic macular edema (DME). These conditions can lead to severe vision loss or blindness if they go undetected. Taking care of your eyes is a top priority when you have diabetes.
Regular Eye Exams
Schedule regular eye exams with an ophthalmologist/optometrist to have your eye health and vision checked. Usually, these exams are scheduled once a year but your doctor might recommend them every six months, based on your health condition. Always wear corrective lenses as needed and follow the advice of your healthcare team. Always wear UVA/UVB sunglasses to help prevent cataracts.
Do You Eat a Healthy and Well-Balanced Diet?
Diet and medication are the cornerstones of diabetes management, along with regular exercise. Eating a healthy, well-balanced diet can help you maintain normal blood sugar levels.
You Are What You Eat
Making smart choices can help you feel energized and avoid blood sugar spikes and swings. Avoid sugary, salty foods. Opt for whole foods over pre-packaged ones. If you are on-the-go, grab a hard cooked egg sandwich and a piece of fruit rather than fast foods. If you want to keep packaged foods on-hand, buy ones that are specifically made for people with diabetes. Select low-fat dairy products rather than whole fat ones. Eat fresh fruit and vegetables or frozen fruit and vegetables without added sugars, salts, and sauces. If you purchase canned fruit or vegetables, read the labels to avoid added sugar and salt. Include lean meats and fish in your diet, such as chicken, turkey, and salmon with heart-healthy omega-3s. Trim the fat off beef such as steak. Buy lean cuts of beef such as loin and try to purchase grass-fed beef. Eating high amounts of beef is “associated with a higher risk of diabetes”. Whole grains are a better choice than white ones. Water and unsweetened tea and coffee are the best beverage choices. Stay away from the empty calories found in soda and sugar-laden juices. Talk to your doctor about taking vitamin and mineral supplements. Make sure you know how they interact with your medications.
Do You Know How to Take Care of Illnesses?
Even if we are proactive about our health, colds and other illnesses can arise. If you are unable to eat and feel sick, contact your doctor about your medication schedule. Always consult with your healthcare team before taking OTC medications as they could have contraindications with your current medications.
Taking Care of Yourself
Your blood sugar levels can rise when you are sick. Adjust your medications in accordance with your doctor’s advice. Test your blood sugar regularly and report highs or lows to your doctor. Be proactive by asking your doctor about pneumonia, shingles and flu vaccinations. Have plenty of sugar-free fluids in the house especially if you have a fever. Make sure to have sugar-free cough medication and sugar-free pain relievers available as well.
Do You Quit Unhealthy Habits?
Unhealthy habits can take their toll on your body, especially when you have diabetes. Defining these habits and eliminating them can make a major difference in your well-being.
Quit the Habit
Women with diabetes should limit their alcohol to one drink daily while men may have two. Excessive alcohol intake can cause blood sugar spikes and other serious health issues. Smoking is another unhealthy habit that can lead to serious illnesses. If you have difficulty quitting these habits, join a support group or talk to your physician about other options. These may include a smoking cessation clinic, a nicotine patch, or hypnosis.
Do You Properly Manage Stress in Your Life?
While it is impossible to eliminate stress from your life, you need to learn how to manage it. Extreme stress can cause your blood sugar levels to soar. Finding ways to manage this stress makes you feel better and face your daily responsibilities with greater enthusiasm.
Stress Relief

If your answer to any of questions above is no, it is time to re-evaluate your diabetes management plan. Talk to your health care team about improving your self-management routine. With the right approach, you can live a happy, healthy life with diabetes.






Leave A Comment