Diabetes remains the leading cause of kidney failure in nearly half of the new cases diagnosed in the United States. Cardiovascular disease is always on the radar screen when you have diabetes, but discussion of kidney disease has limitation. According to the findings in The Journal of Diabetes, “Among adults with type 1 diabetes, those with higher A1Cs and elevated blood pressure numbers, are more likely to develop kidney disease.” Glucose control, “across the life span” remains critical, reduces future long-term diabetes complications, especially kidney disease. According to Clinical Journal of the American Society of Nephrology, “mortality among those with kidney failure in the US has significantly decreased between 1995-2013.” This shows with all reasons for kidney failure including those on dialysis and with a kidney transplant.
Almost 2 million people have been in this study. This is certainly good news! Early kidney changes, also known as microvascular disease, shows only 2-3 years into a diabetes diagnosis; treatment should start early. Kidney disease’s progression to kidney failure takes approximately 20 years in type 1 diabetes and 10 years in type 2 diabetes; stopping the progression is the goal. Discover more about diabetes kidney disease, dialysis, kidney transplants and new trends.
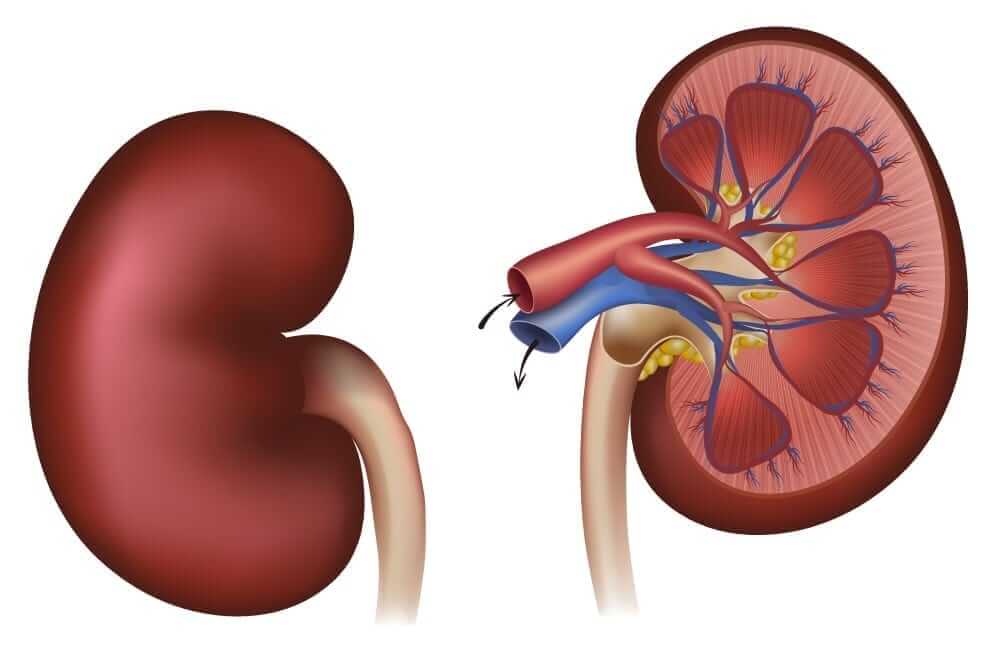
Kidney Function Basics
The kidneys filter toxins, waste products, drugs, food, glucose and excess fluid from the bloodstream and puts them into the urine for excretion. They also filter blood before sending it back to the heart. The kidneys promote bone health, produce red blood cells and help regulate blood pressure. The most important part of the kidney are the nephrons; each kidney has approximately 1 million nephrons. With diabetes, blood sugars which are continuously elevated, cause excess sugar in the system; this can affect functions of kidney nephrons and tiny blood vessels. The kidneys become less efficient, their abilities decrease, and toxins build up. 20-40% of people with diabetes- both type 1 and 2, will eventually develop chronic kidney disease (CKD) if blood sugar and blood pressure is not controlled.
What About Kidney Disease?
As stated above, it can take many years for kidney disease to develop when you have diabetes. In the beginning, small amounts of a blood protein called albumin leak into the urine. Typically, the kidneys continue to filter normally during this first stage of kidney disease called micro-albuminuria. Over time, more albumin gets into the urine and the ability for the kidneys to filter decreases. This stage called proteinuria or macro-albuminuria. The body starts to retain wastes and kidney damage occurs as a result of this lack of filtration. Not everyone with diabetes develops kidney disease; people with diabetes for over 25 years with no signs of kidney problems have a lower risk of developing kidney disease. Those who maintain good blood sugar and blood pressure control have an extremely reduced chance of developing kidney disease, even after many years of diabetes.
Kidney Disease and Diabetes Statistics
There are about 29 million people in the United States with diabetes and nearly 300,000 of them have kidney failure. Most people with diabetes may have CKD, but do not experience kidney failure, which is the final stage of CKD. It occurs when the kidneys “fail to get rid of body waste.” When people have uncontrolled diabetes, it can cause injury to small blood vessels in the body. If these blood vessels are in the kidneys, they are unable to properly clean the blood. Early treatment and diagnosis should begin before kidney damage can occur.
Common Risk Factors for Kidney Disease
- women have more early stages of chronic kidney disease, but men develop higher rates of kidney failure
- years of elevated A1C levels
- chronic uncontrolled hypertension
- older age
- family history of kidney disease
- length of diabetes
- race/ethnicity- Mexican, Native and African American have higher incidences of CKD
What Are the Possible Symptoms of CKD?
At the beginning you may experience:
- swollen ankles
- hypertension
- weight gain
- shortness of breath
- protein in the urine
- increased nighttime urination
- trouble sleeping/distracted concentration
As kidney disease progresses:
- increased albumin levels
- foamy urine
- severe leg cramps
- swollen face, puffy eyelids
- anemia
- abnormal glomerular filtration rate (GFR)- blood test
And finally, CKD stage 5: kidney failure
- a metallic taste/bad breath
- uremia- (toxins in the blood stream)
- nausea and vomiting/ loss of appetite
- profound weakness/pallor
- severe itching
Diabetes can also cause nerve damage. This makes it harder to empty your bladder. A full bladder backs up and can lead to injury of your kidneys. Urine with high sugar levels that stays in the bladder can lead to infections due to the quick growth of bacteria. This condition may also lead to CKD.
What About High Blood Pressure and Other CKD Causes?
People with diabetes, especially type 2, are more likely to have high blood pressure. The leading cause of kidney failure is diabetes and the second most likely cause of kidney problems is high blood pressure. Use a blood pressure monitor daily and report irregularities to your health care team. Other causes of kidney disease include heart problems, alcoholism, hepatitis C and HIV.
Medical Monitoring Matters- What Can I Do?
The first thing you can do yearly is have a complete physical and history exam. Discuss any of the symptoms listed above, which may indicate kidney problems. People with diabetes should also get a kidney screening at least once a year. Talk to your doctor about scheduling one. If detected of having kidney disease, then patients should visit with a kidney specialist called a nephrologist.
Consult with a dietician specializing in kidney disease need arranging. Suggest in a “kidney friendly diet.” It may include whole fruits and vegetables in moderation. Avoid foods high in potassium and phosphorous such as bananas, oranges and avocados. Total daily protein may need reduction, but high-quality protein needs to remain in your eating plan. Cutback on Sodium or salt since it can disrupt the mineral balance in your blood and make you retain fluids. Avoidance of canned goods (soups, sauces, beans) and vegetables (heavy in salt). If severe weight loss is a problem, then suggest enough high-quality calories. Removal of some whole grains such as brown rice and whole wheat since they contain high levels of phosphorous and potassium.
Limit or eliminate sugary foods and alcohol. You may need to limit total fluids as well. Lose weight if you are overweight or obese. Incorporate good eating habits for your diabetes, at the same time.
Ask your doctor to help you be proactive about kidney disease by routinely measuring your A1C levels. You should be checking at home as well with a glucose meter or continuous glucose monitor. Monitor your kidney blood work- GFR, BUN and creatinine levels. Know what numbers your doctor is looking for.
Your blood pressure should be checked during every medical examination and at home. Know what number you need. Most physician’s want to maintain blood pressure below 140/80-90, depending on your personal situation. Work with your health care team to minimize a potential kidney disease leading to failure.
You may require imaging tests of the kidney which includes an ultrasound. This can show kidney structure and size. Other common tests may include a CT/MRI which can show blood flow to the kidneys. Finally, a recommendation to do a kidney biopsy.
Avoid medical tests that require contrast dye; filtered contrast dye thru the kidneys and may cause kidney shut down if they are not functioning well. Heart angiograms and certain CT scans require contrast dye.
Lower your cholesterol levels; usually your doctor will add statin medications if you are not already on them. Dietary changes and weight loss may also be recommended.
Treat urinary tract infections quickly. If they are not treated and progress to the kidney, there will be more damage. Talk to your physician about having antibiotics on hand to treat infections early.
Your medications may need changing if filtered thru your kidneys. Talk to your physician. A new guideline set by the ADA, that your physician should be aware of that, “you can now continue metformin, an old diabetes drug until your GFR is 30ml/min or less.” Taking an ARB or ACE inhibitor for your blood pressure can also help protect your kidneys. New research shows that SGLT-2 inhibitors- which pull sugar out of the urine, including Jardiance or Invokana, protect and enhance kidney outcomes in those with diabetes. Take your diabetes medications as prescribed to help keep your blood sugar levels regulated.
Meet with a diabetes educator-CDE, you can review all aspects of diabetes care and know the possible additional complications of the disease.
Avoid OTC pain killers such as Advil, Aleve, Motrin and Naproxen. They may cause additional kidney damage.
Exercise daily by doing aerobics such as walking, biking, and swimming to help lower your blood pressure. Consider yoga practice and Thai Chi for mental and physical health.
Find ways to minimize stress, including relaxation techniques such as deep breathing exercises or biofeedback.
Do not start smoking and quit if you do smoke.
What Is Dialysis?
There are 5 stages of kidney disease and once chronic kidney disease leads to Stage 5, called, ” kidney failure”, recommended to do a dialysis. Dialysis is a way to artificially clean the blood of waste products and toxins. It removes the extra fluid and accumulated wastes from your blood. Dialysis may cause anemia, infection and nerve damage in some patients. During dialysis, your blood pumps through tubes to a dialysis machine. The treatments take about 3 to 5 hours and usually done 3 times weekly. Commonly at an out-patient dialysis center, in a hospital setting, or in your own home.
If done at home, requirements include adequate space, electric power, and water drainage to operate the unit as well as a care partner. There are 3 basic types of home dialysis including conventional, short daily home dialysis, and nocturnal dialysis while you sleep. Discuss your options with your health care team to choose the right one for your situation. Dialysis treatment has vastly improved over the last decade along with the results.
Kidney Transplants
Although not for everyone, some people with kidney failure may qualify for a kidney transplant. Dialysis takes a lot of time, is labor intensive and may take a huge emotional toll; a kidney transplant can free you from dependence on dialysis. Kidney transplant patients also live longer than dialysis patients; they tend to have less diet restrictions, have more energy and a better sense of well-being. “Life expectancy can be from 8-20 years after a transplant.” After you and your doctor decide you are a potential candidate, evaluated you by a transplant center. You will meet with a social worker and psychologist since an organ transplant requires certain future lifestyle changes. A kidney transplant is a, “surgical procedure that is done to treat kidney failure.” Which will place a donated kidney into your body.
Kidney transplant from a live donor will provide the best scenario for you; it can be from a family member or other live donor, but the blood type and tissues must match. If that is not possible, you will have a placement on an Organ Procurement and Transplantation Network (OPTN) list; the usual wait time for a deceased kidney is 5 years.
After the transplant you will need to take immune-suppressing drugs for life, to keep your immune system from attacking the new kidney. Things have improved in the world of kidney transplants since there is now better access, longer survival rates, improved medical care and newer medications. On the other extreme, finding suitable kidneys for all patients who need one is still an impediment. Organ donation needs to be a part of more peoples ‘ involvement. Think about signing organ donation cards and checking the box on your driver’s license if you can be a possible donor.
Finally
Maintaining proper blood sugar levels and blood pressure control can help people with diabetes avoid kidney disease and failure. For those who experience kidney disease, healthy lifestyle habits and ongoing treatment can make a difference. Talk to your health care team today about kidney disease and how you can minimize its potential impact on your life.






Leave A Comment