Diabetes management often involves self-administration of insulin to avoid severe blood sugar fluctuations. It can be frustrating to inject several insulin shots a day without achieving proper glucose control. Insulin pumps are used to provide a more consistent amount of insulin through out the day and night which allows for added flexibility. Find out the specifics about how to use an insulin pump and what it can do for you.
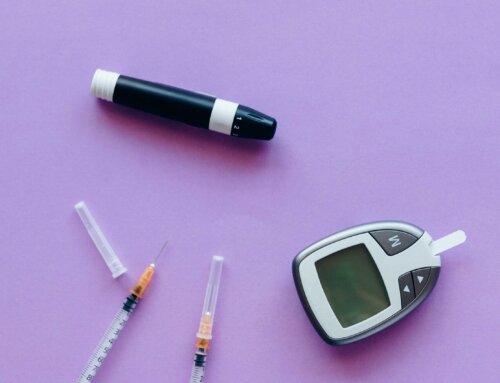
- An insulin pump provides a continuous flow of rapid-acting insulin that is released into your body through a small, flexible tube called a catheter. The catheter is inserted through a needle under the skin usually by your abdomen then taped to stay in place. The amount of insulin administered can be changed by the user. An insulin pump administers continuous insulin 24 hours a day rather than taking multiple insulin injections that may cause blood sugar fluctuations. It can also give a burst of insulin (bolus) if the blood sugar is high.
- Health care providers may recommend using an insulin pump to mimic the slow release of insulin similar to a normal functioning pancreas. Some studies show the pump may provide better blood sugar control that multiple daily insulin injections and improve A1C values. Using a pump frees people with diabetes from having to measure insulin into a syringe or carry an insulin pen as well as experiencing frequent needle sticks. You should monitor your blood sugar levels at least 4 to 6 times a day. Based on your exercise program and food intake, you will set the doses of insulin and make necessary adjustments on your pump.
- Your health care provider will discuss the unique programmed plan for your insulin pump. A experienced pump trainer will teach you all the pump specifics and will continue to be an available support person. Between meals and overnight, a small amount of insulin is delivered through the pump to keep your blood sugar in a target range. This is referred to as the basal rate. When you eat, a bolus dose or burst of insulin can be programmed into your pump. The amount of bolus you need can be measured by calculating the grams of carbohydrates you will eat. This is similar to how the normal functioning pancreas works.
- An insulin pump is designed for convenience but you must use it properly. Your doctor or pump trainer will help you get accustomed to using it. Many hospitals have an out-patient program to help you get comfortable using and setting the pump. Many pump companies supply free pump training classes as well. You may also have a one-day hospital stay to learn how the pump works. Your health care team will use training time to discuss effective diabetes self-management.
- Maintain a daily record of your insulin pump flow rate and blood glucose levels to help you make necessary adjustments. Review these records weekly to note patterns of abnormally low or high glucose levels. Discuss the results from your daily diary with your health care provider at regular appointments. Contact your doctor immediately about abnormal highs and lows.
- Your insulin pump can be disconnected for a short time but no more than two hours. In case you are unable to use your insulin pump, travel with extra supplies and insulin pen to avoid severe blood sugar fluctuations.
- Potential disadvantages of using an insulin pump include weight gain due to the body handling carbohydrates more efficiently and possible expense. You will need to replace the catheter every 3 days for proper use. Sometimes a catheter can dislodge and you will not get accurate doses of insulin. Having injections or an insulin pen on hand is always needed for emergencies. Many patients find the advantages outweigh the possible disadvantages.
Insulin pumps are often an easier way to self-manage diabetes than multiple daily injections. Talk to your doctor about insulin pumps and whether they are a good choice for you. With proper training, insulin pumps give people with diabetes greater blood glucose control and more personal freedom.





Leave A Comment