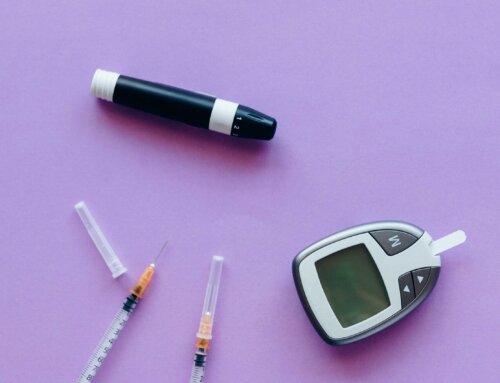
People with diabetes who use insulin traditionally use a vial-and-syringe method for delivery. An insulin pen has become another alternative for delivering insulin. Find out more about the advantages and disadvantages of insulin pens.
How Insulin Pens Work
Insulin pens have an attached insulin cartridge rather than using a syringe and separate vial. Pens contain cartridges that last somewhere between 2-4 weeks and must be disposed of after expiration or when empty. Insulin pens require insulin pen needles that are replaceable and need to be changed and disposed of after each injection. Pen needles are usually thin and short, between 4-6 mm, for optimum comfort. There is no need to pinch up the skin with these shorter needles; just inject straight into the skin. If you are using longer pen needles between, 8-12.7 mm, then you need to pinch up the skin to prevent injecting the insulin directly into muscle. Most pre-filled pens must be discarded within 14-40 days depending on the insulin type. Patients should always verify the time frame with the package insert as brands will vary. If the insulin pen you are using contains 2 different types of insulin, you must roll the pen back and forth to mix the two insulins before each injection. Never use insulin that contains floating particles or clumps inside the cartridge. Remember, with any insulin, the injection site must be rotated each time.
Ease of Use
Patients report an easier overall injection experience when using an insulin pen. Pens tend to be more socially friendly because they are smaller and less noticeable than the classic vial-and-syringe. Insulin pens are more portable for people on-the-go. Pens that are open do not need to be refrigerated and can be thrown into a pocket or purse for easy travel. Room temperature insulin tends to be absorbed better. Pens are user-friendly when patients get specific instruction from a doctor, diabetes nurse educator or pharmacist. This training usually takes less time than teaching someone how to use a vial-and-syringe. Also, the recent introduction of safety needles has been helpful for patients who are anxious about using needles.
Cost Versus Accuracy
Often the prescription cost for pre-filled insulin pens is higher than the cost of insulin vials. This depends on what a patient’s insurance covers. Certain insurance providers and Medicaid may require prior authorization for the use of insulin pens. A separate prescription is required for the pen needles. Some patients find the accuracy associated with insulin pens helps them save money because less insulin is wasted. Users must remember insulin may still be released by the pen for several seconds after it is fully depressed. The patient must wait for about 6- 10 seconds with the pen needle remaining in the skin to ensure the insulin is fully absorbed.
Visually Impaired and Elderly
A pen might be easier for visually impaired people to use, as well as those with reduced dexterity. The numbers stamped on insulin pens are larger than the ones on syringes, which make them easier for people to see. Because there is no syringe to be filled, it can be easier for elderly people or those with minimal dexterity to use a pen. People with visual problems should use a pen that has a clear screen with clicks that are easy to hear to ensure the proper dosage is administered. People with minimal range of motion in their hands may find it difficult to use a pen, as some pens require more force than others. The magnitude of the condition of each patient determines whether the pen is a viable solution.
Priming an Insulin Pen
Pens need to be primed prior to each injection. Remember the needle must be removed after every use to prevent air in the insulin. The patient needs to dial up 2 units and inject them into the air called an “air shot” for an accurate injection. Insulin pen cartridges come with extra insulin in consideration of this “air shot.” Patients must remember to do this every time until they observe a steady stream of insulin coming out of the pen. All insulin pens, whether short or long acting insulin, need to be primed.
Recent studies have revealed insulin pens are underused in the United States, despite the fact they are associated with greater A1C improvement and lower claims for hypoglycemia. The cost and insurance coverage are factors associated with the current lack of use. Talk to your doctor to find out whether an insulin pen might be a good solution for you.






Leave A Comment