Taking care of the skin and scalp you’re in matters even more when you have diabetes. People with diabetes are at higher risk for many skin complications. Following basic skin care tips helps you minimize those risks.
- People with diabetes have an increased risk of dry skin and skin infections. They are prone to bacterial and fungal skin infections such as styes, boils, folliculitis, carbuncles, nail infections, jock itch, athlete’s foot, ringworm and yeast infections. About one third of people with diabetes have skin problems.
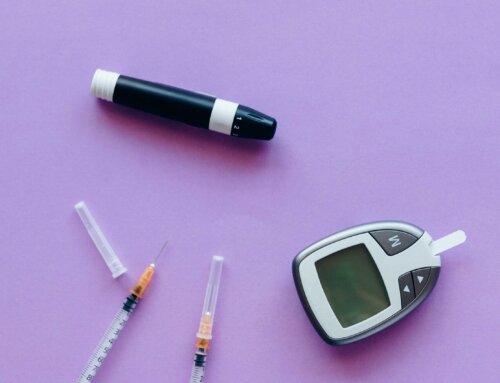
- Fluctuating glucose levels increase your risk of developing skin conditions. Make sure to test your blood sugar regularly and keep it in target range. When you use alcohol swabs to test with blood glucose meters, it may cause dryness and irritation. Wash with soap and water instead then dry hands completely before testing (you may use alcohol or an alcohol based gel if no soap and water is available since it is always recommended to have clean hands prior to testing).
- Visit a dermatologist every year for a head-to-toe checkup. Early detection of skin conditions is crucial to avoid complications such as ulceration, gangrene and possible amputation.
- Vitiligo is an autoimmune disease associated with type 1 diabetes that affects skin coloration. Special cells that make pigment are destroyed causing patches of discolored and lightened skin. Vitiligo typically affects the abdomen, chest, hands and face. Treatments include micro pigmentation and topical steroids. If you have vitiligo, use a sunscreen with an SPF of 15 or higher to avoid getting sunburn on the discolored skin areas. Wear a hat to cover your head as well and consider SPF treated clothing.
- Alopecia is another autoimmune disease associated with type 1 diabetes that results in hair loss. The cause of alopecia is unknown. Hair loss can occur on the scalp or other areas of the body. Check with a physician for best treatment.
- Dry skin can be related to neuropathy and poor circulation. This may cause the sweat glands to slow or shut down. Without sweat to maintain moist skin, further dryness occurs. This can result in severe cracks in the skin especially in the feet leading to fungal infections such as athlete’s foot. Toenail fungus is also very common. To keep feet healthy, apply diabetic foot creams and wear breathable and anti-bacterial diabetic socks.
- Acanthosis nigricans is the development of darkened skin at the back of the neck, groin, underarms, elbows and knees. Acanthosis nigricans can be a sign of insulin resistance. Children with type 2 diabetes and people who are obese often develop this skin condition. Minorities such as Hispanics are at higher risk as well.
- Always keep your skin clean, dry and moisturize as often as possible. Try to moisturize after the bath or shower when skin is already damp. Take care of wounds immediately by washing with soap and water, using an antibiotic ointment and covering them to avoid infection. Consult a physician immediately if you suspect an infection. If you have diabetic neuropathy, you might not feel a wound or irritation. Check your skin, including the soles of your feet regularly to keep them in good shape.
- Drink water to keep your skin hydrated from the inside out. Be aware of irritants that cause infection. Use lancets only once. Rotate sites for injections with insulin syringes and rotate fingers for pricking. Use caution outdoors. Wear sun block when you are exposed to the sun even when it is cloudy or overcast. Watch out for bug bites and treat them immediately.





Leave A Comment